The journey towards revolutionizing stroke care through technology is both exhilarating and fraught with economic complexities. As healthcare systems worldwide grapple with the rising tide of stroke-related disabilities, the allure of cutting-edge technologies offers a beacon of hope. These innovations promise not only to enhance patient outcomes but also to streamline the labyrinth of stroke management processes. Yet, the path to their integration is not without its financial hurdles. This blog delves into the economic challenges inherent in adopting new stroke care technologies and navigates through potential solutions that aim to harmonize clinical excellence with fiscal prudence.
The Economic Burden of Stroke Care
Stroke remains a leading cause of disability and places a significant economic burden on healthcare systems worldwide. The cost associated with post-stroke care (PSC) is staggering, with figures showing the highest expenditure in countries like the USA, where inpatient and outpatient PSC costs can reach up to $4850 per patient month (PM) (Rajšić et al., 2018). Such financial strains call for an urgent need to find more cost-effective solutions in stroke management.
The Economic Costs of Futile Transfer Costs
An often overlooked aspect of economic challenges in stroke care is the cost associated with futile patient transfers. Transferring stroke patients to facilities equipped for advanced care, only to find that they are not suitable candidates for procedures like mechanical thrombectomy, incurs substantial unnecessary costs. These costs stem from ambulance services, emergency department resources, and the opportunity cost of occupying medical facilities that could otherwise serve patients in need. Developing more accurate pre-hospital assessment tools and protocols, facilitated by telemedicine, could mitigate these costs by ensuring that only patients who are likely to benefit from advanced interventions are transferred (Martinez‐Gutierrez et al., 2019).
The Financial Quagmire of Adopting New Technologies
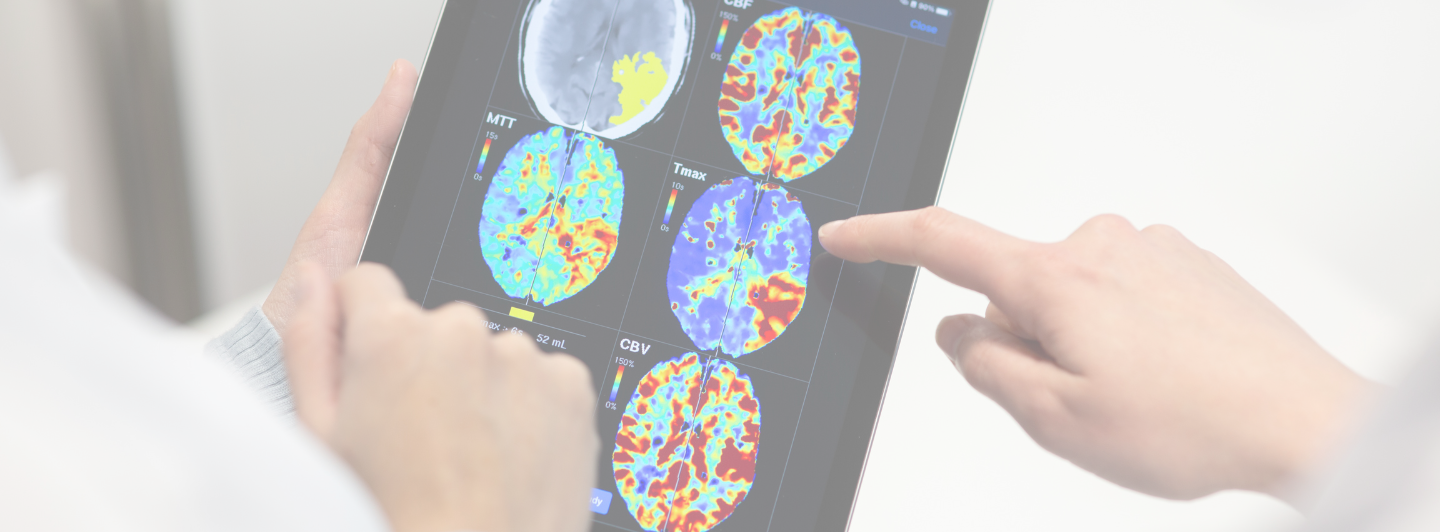
The adoption of advanced technologies in stroke care introduces a financial conundrum for many healthcare providers. Initial costs for state-of-the-art equipment, training healthcare personnel, and integrating new systems into existing infrastructure can be daunting. Additionally, the uneven distribution of medical resources across regions exacerbates the challenge, making it difficult for patients in rural or underserved areas to access these lifesaving innovations (Wu et al., 2020). Furthermore, the economic burden of stroke care is compounded by post-stroke rehabilitation and nursing care, which are pivotal in patient recovery but require substantial investment (Rajšić et al., 2018).
A pivotal challenge in adopting new stroke care technologies lies in the disparity of access across different regions, especially in low-income and middle-income countries (LMICs). The burden of stroke is notably higher in LMICs, where the integration of advanced stroke care services is hampered by economic constraints, insufficient healthcare infrastructure, and a lack of trained healthcare professionals (Pandian et al., 2020). Furthermore, the initial costs associated with the procurement and implementation of advanced technologies, such as telemedicine and mobile stroke units, present substantial financial barriers for many healthcare systems.
Solutions to Economic Barriers
Addressing these economic barriers requires innovative financing models and international cooperation. For instance, implementing cost-sharing mechanisms, securing grants from international health organizations, and fostering public-private partnerships can provide the necessary funding for technology adoption. Moreover, developing scalable and adaptable technology solutions can ensure that investments in stroke care technologies yield long-term benefits across various healthcare settings. Training and capacity building, particularly in LMICs, are also essential to ensure the effective use and sustainability of new technologies (Bagot et al., 2018).
Moreover, adopting a phased implementation strategy can help mitigate upfront costs, allowing healthcare facilities to scale up based on success rates and financial viability. The development of telestroke networks is a testament to how technology can overcome geographical and financial barriers, providing remote consultation services that extend the reach of specialized stroke care to underserved areas (Bagot et al., 2018).
As healthcare systems evolve, the integration of technological innovations in stroke care stands as a pivotal milestone towards achieving equitable, efficient, and effective treatment for all. Overcoming the economic challenges requires a concerted effort among stakeholders, innovative thinking, and a commitment to redefining the standards of care. The journey ahead is complex, but the potential rewards for patients and providers alike are immeasurable.
In the spirit of innovation and with an eye towards the future, the role of solutions like Strokeviewer cannot be overstated. As we explore the economic facets of stroke care technology adoption, it becomes clear that platforms such as Strokeviewer offer not just a glimpse into the future of healthcare but a tangible pathway to overcoming some of the most pressing challenges faced today.
Stay tuned for our upcoming series, “How AI Diagnostics and Collaborative Tech Tools Contribute to Cost-Saving in the Healthcare Systems” and discover the pivotal role technology plays in not just enhancing patient care but ensuring it’s financially accessible to those who need it most.
Interested in how Strokeviewer can transform your Stroke Team? Scheduling a demo might just be the step forward you’re looking for.