In a sector where every moment counts, the significance of reducing time-to-treatment in healthcare settings brings with it an urgency that is not only a matter of life and death but also of economic concern for all parties involved—healthcare providers, insurers, and patients. This exploration seeks to untangle the complex web of financial implications tied to the timeliness of medical interventions, bolstered by insights from the latest research.
The Economic Essence of Timeliness
Timeliness in healthcare delivery is a critical factor that influences not just clinical outcomes but the economic landscape of health services. Delayed interventions, particularly in acute conditions like strokes or heart attacks, can dramatically affect the trajectory of patient recovery and the associated costs. The financial impact of these delays touches every corner of the healthcare system, from altering hospital revenue streams and insurance payouts to burdening patients with heavier out-of-pocket expenses.
An often overlooked but critical aspect of reducing time-to-treatment and its associated costs is the role of AI in diagnostics, particularly in preventing unnecessary transfers of stroke patients from spoke hospitals to hub hospitals. Unwarranted patient transfers not only strain healthcare resources but also impose significant financial burdens on both healthcare systems and patients. The costs associated with ambulance services, emergency department utilization at hub hospitals, and the potential for longer hospital stays due to transfer-related delays can accumulate rapidly. AI diagnostics, like those offered by Strokeviewer, have the potential to revolutionize this aspect of stroke care. By providing rapid, accurate assessments of stroke imaging at the point of care, these AI tools empower spoke hospitals to make informed decisions about the necessity of patient transfers. This capability can lead to substantial cost savings by eliminating unnecessary transport and treatment expenses, optimizing resource allocation across the healthcare network, and focusing hub hospital resources on patients who truly require specialized care. Moreover, by minimizing unwarranted transfers, patients are spared the stress and potential risks associated with long-distance transportation, contributing to better overall patient experiences and outcomes. In this way, AI diagnostics not only streamline the patient care pathway but also introduce significant economic efficiencies into the stroke care continuum.
Financial Impact on Healthcare Providers
Reducing time-to-treatment has a direct correlation with hospital operation costs and overall financial performance. A study investigating the financial impact of minimizing door-to-balloon time for ST-elevation myocardial infarction patients revealed that while hospital revenues from insurance payments decreased, so did the total hospital costs, leaving the net income per admission relatively unchanged. This finding underscores the financial viability of improving treatment timelines, as the decrease in operational costs offsets the drop in revenue, maintaining the hospital’s financial health (Khot et al., 2009).
The economic valuation of care significantly escalates with prompt intervention—each 10-minute advancement in treatment delivery amplifies the net monetary benefit (NMB) by approximately $10,593 to $10,915 from healthcare and societal perspectives, respectively. This data poignantly highlights the dual advantage of timely treatment: enriching patients’ lives with more disability-free days while simultaneously fortifying the economic efficiency of healthcare delivery (Kunz et al., 2020).
Financial Impact on Patients
In the nuanced ecosystem of stroke care, the economic burden that delayed treatment places on patients illuminates the critical nature of timely medical intervention. Beyond the face value of immediate healthcare expenditures, the domino effect of postponed treatment unfolds in the form of escalated indirect costs—including lost wages and extensive rehabilitation expenses. Crucially, patients afforded prompt access to treatment not only benefit from shorter hospital admissions but also from accelerated recuperation periods, significantly alleviating financial pressures. Early intervention stands as a bastion against the progression of medical conditions, potentially circumventing the necessity for more sophisticated, costlier treatments and thereby securing substantial savings for patients.
Recent findings further quantify the tangible benefits of expedited treatment, revealing that each 10-minute reduction in treatment delay correlates with an average gain of 39 disability-free days, offering patients a more prolonged period of quality life (Kunz et al., 2020). This research underscores a pivotal economic revelation: while the aggregate lifetime costs borne by patients receiving either timely or delayed treatment converge to a similar financial endpoint, the path diverges markedly in terms of quality of life and healthcare utilization. Specifically, delayed treatment culminates in heightened morbidity-associated expenses, albeit condensed within a briefer lifespan.
Financial Impact on Insurers
The integration of AI diagnostics in stroke care also presents significant implications for insurers, who play a pivotal role in the healthcare ecosystem. By reducing unnecessary patient transfers and optimizing the allocation of healthcare resources, AI diagnostics can lead to lower claims costs for insurers. This decrease is primarily due to the reduction in expensive emergency transport services, minimized use of high-cost hospital resources, and potentially shorter hospital stays resulting from expedited treatment initiation. Furthermore, as AI-enhanced diagnostics contribute to more accurate and timely treatment, patients are likely to experience better health outcomes, which can further reduce the long-term costs associated with post-stroke care and rehabilitation. Insurers might also see an opportunity in these technologies to enhance the value of their coverage offerings, improve patient satisfaction, and promote a more sustainable healthcare model by supporting policies that favor the adoption of cost-saving and outcome-improving technologies like AI diagnostics. Ultimately, the widespread use of AI in stroke care could foster a closer collaboration between healthcare providers and insurers, aimed at achieving a common goal: high-quality, cost-effective patient care.
Strategies to Reduce Time-to-Treatment
Implementing strategies to expedite patient access to necessary medical interventions involves both technological and procedural enhancements. Telemedicine and digital health platforms, for example, have shown promise in reducing pre-hospital delays, enabling quicker diagnosis and treatment initiation. Streamlining hospital protocols and enhancing coordination between emergency and specialty departments are also vital steps toward minimizing treatment delays.
Role of Technology in Optimizing Time-to-Treatment
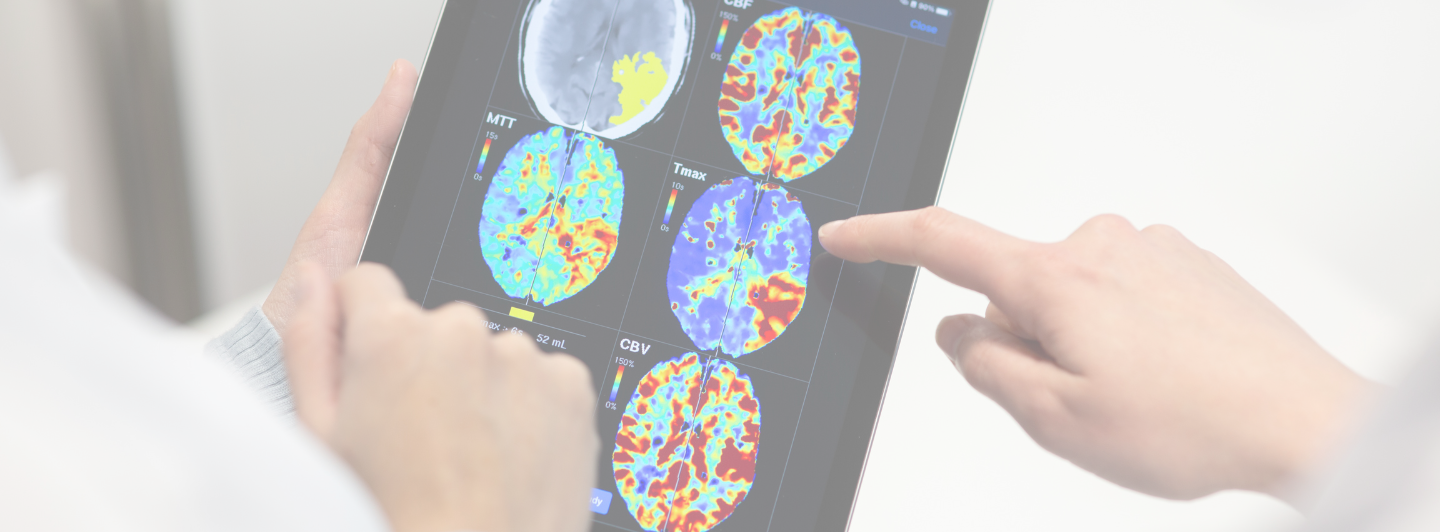
Innovations in healthcare technology, particularly those leveraging artificial intelligence (AI), play a pivotal role in reducing time-to-treatment. AI-driven tools, such as Strokeviewer, offer the potential to dramatically accelerate the diagnosis and treatment planning process for stroke care. By enabling faster and more accurate analysis of medical imaging, these technologies assist healthcare providers in making swift, informed decisions, ultimately reducing the time from hospital admission to treatment initiation.
The quest to reduce time-to-treatment not only aligns with the clinical goal of improving patient outcomes but also presents a financially prudent approach for healthcare providers and a cost-saving avenue for patients. As healthcare continues to evolve, leveraging technological advancements such as AI will be instrumental in achieving these time-sensitive treatment objectives.
For healthcare professionals dedicated to the forefront of stroke care innovation, the integration of technologies like Strokeviewer marks a significant stride toward optimizing treatment timelines and enhancing patient care, all while navigating the financial complexities of healthcare delivery.
In the journey towards more efficient stroke care, Strokeviewer stands as a testament to the power of technological innovation. By equipping stroke teams with AI-powered diagnostics and advanced DICOM viewers, Strokeviewer enables physicians to access and share crucial patient information swiftly, anywhere and anytime. This capability is instrumental in enhancing care coordination and reducing time-to-treatment, aligning both clinical and economic interests.
Looking Ahead
As we continue to probe into the economics of healthcare innovation, the forthcoming “Funding and Investment Trends in Stroke Care Technology” series will delve into the financial engines propelling advancements in stroke treatment. How will emerging funding models and investments influence the adoption of groundbreaking technologies in stroke care?
For healthcare professionals keen on harnessing the potential of AI to refine stroke care, scheduling a demo of Strokeviewer offers a gateway to understanding how this cutting-edge technology can transform patient outcomes and economic efficiency alike.